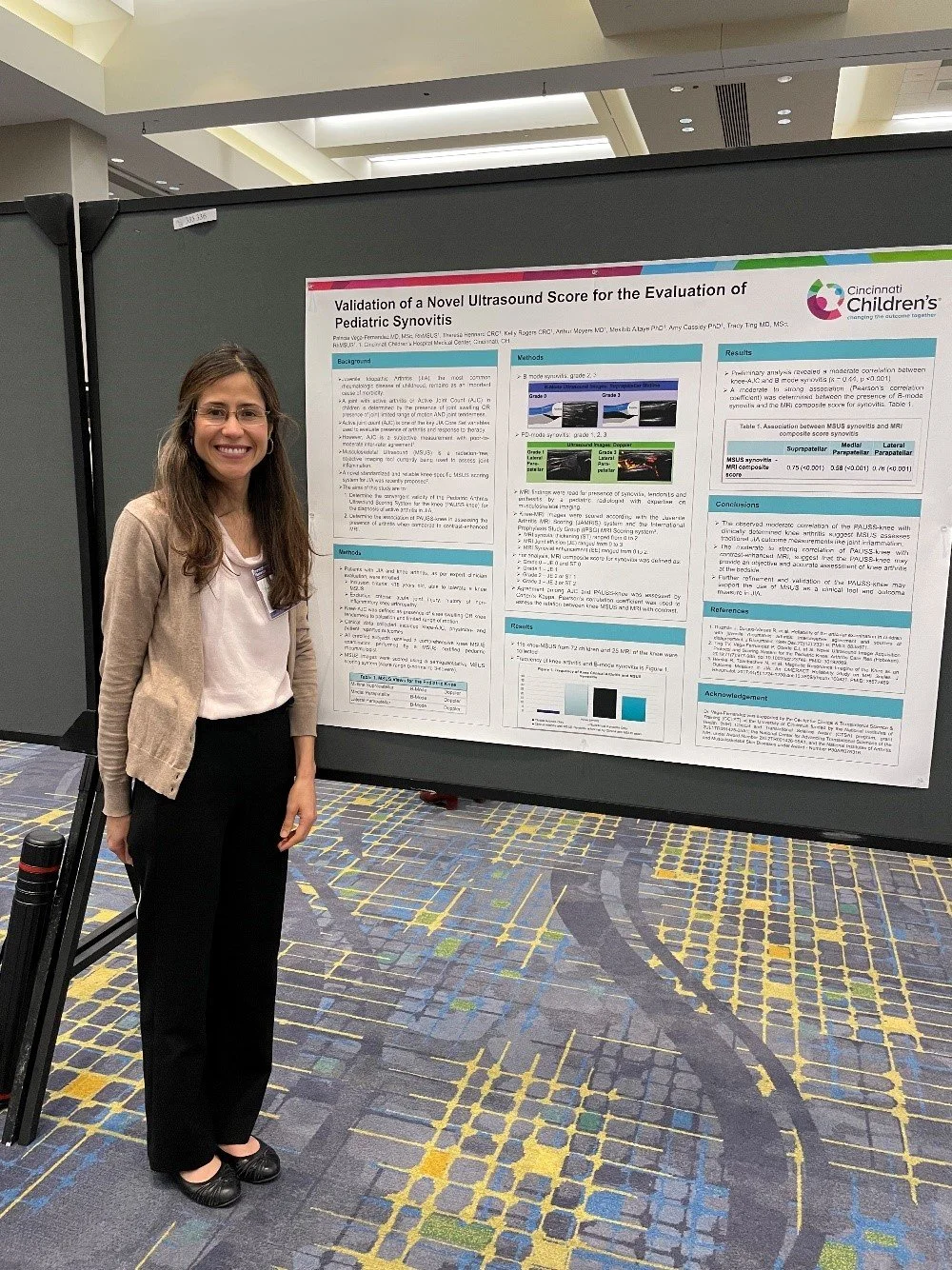
Dr. Patricia Vega Fernandez pictured presenting poster at ACTS conference
KL2 program graduate Patricia Vega Fernandez MD, MSc, RhMSUS, assistant professor in the Division of Rheumatology, Cincinnati Children’s Hospital and K Scholar Natalja Stanski, MD, assistant professor in the Division of Critical Care Medicine, Cincinnati Children’s Hospital presented posters of their research at the annual Association for Clinical and Translational Science (ACTS) meeting.
Dr. Vega-Fernandez’s project is titled, Validation of a Novel Ultrasound Score for the Evaluation of Pediatric Synovitis.
Juvenile Idiopathic Arthritis (JIA), the most common chronic rheumatic disease in childhood, causes substantial morbidity worldwide. Diagnosis of arthritis in children is based on the presence of joint swelling and limited range of motion and/or tenderness on palpation. However, clinical detection of active arthritis in the developing skeleton has limited agreement even if performed by an experienced clinician. Ultrasound (US) is a non-invasive and accessible diagnostic modality that is often the first-choice imaging examination in pediatrics. The objective of this study is to validate a novel Pediatric Arthritis US Scoring System (PAUSS) for the assessment of knee arthritis in JIA. The validation of the knee-PAUSS will facilitate medical decision-making process to timely diagnose and most effectively and safely treat arthritis and to improve the outcomes of children with JIA.
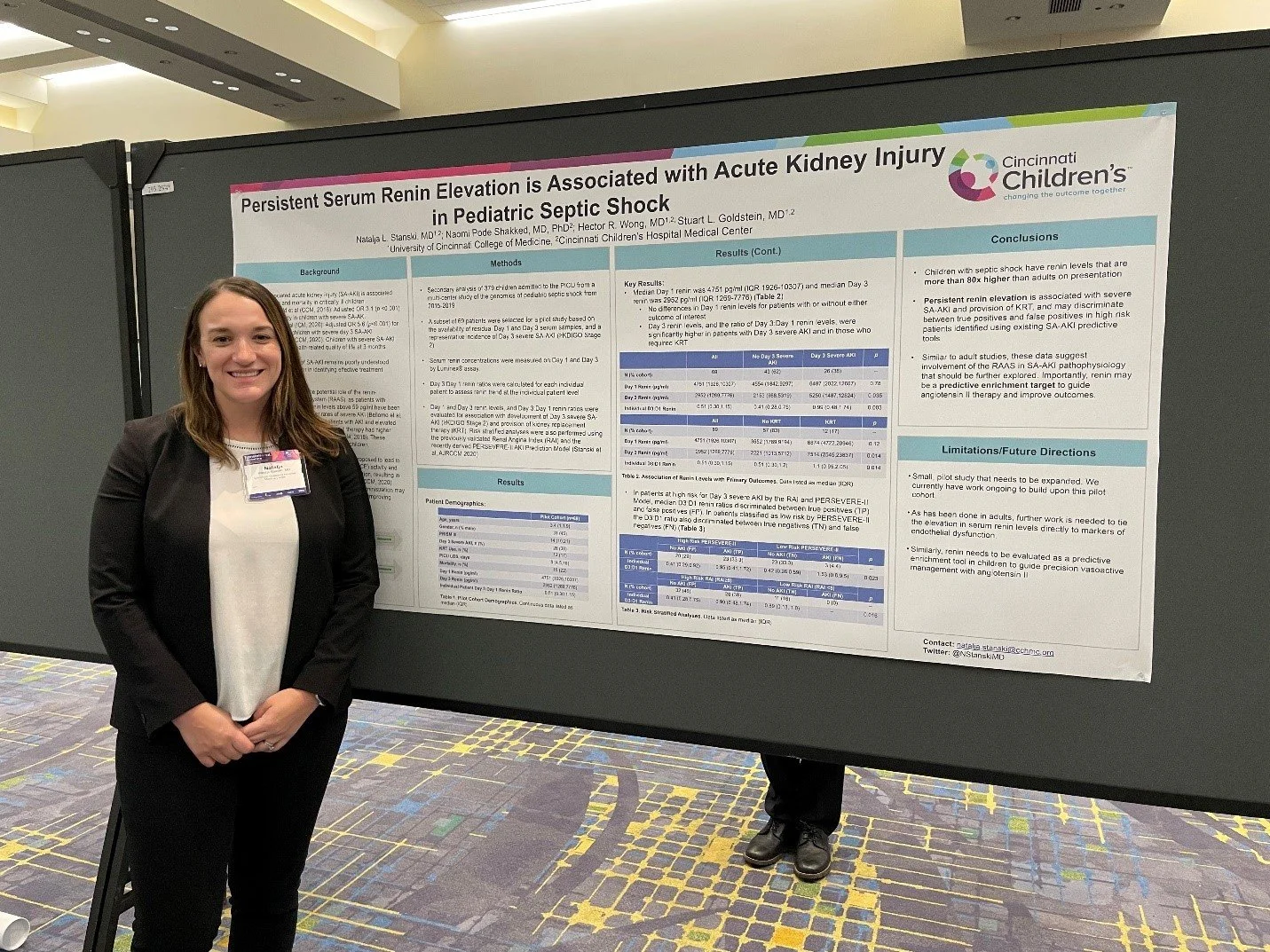
Dr. Natalja Stanski pictured presenting poster at ACTS conference
Dr. Stanski’s project is titled, Persistent Serum Renin Elevation is Associated with Acute Kidney Injury in Pediatric Septic Shock.
Dr. Stanski’s project examined the association between serum renin levels- a marker of renin-angiotensin-aldosterone system dysregulation- and the development of severe sepsis-associated acute kidney injury in a cohort of children with septic shock. She found that children with septic shock had very elevated serum renin levels on admission, and children who continued to have high levels at day 3 were more likely to have severe acute kidney injury and require renal replacement therapy. She also found that this trend in serum renin levels helped distinguish between true positives and false positives identified using her previously published sepsis-associated acute kidney injury prediction model that she is working to prospectively validate as part of her CT2 project. This small pilot study is the first to describe this association in critically ill children, and she is currently working to expand this work to a larger cohort.